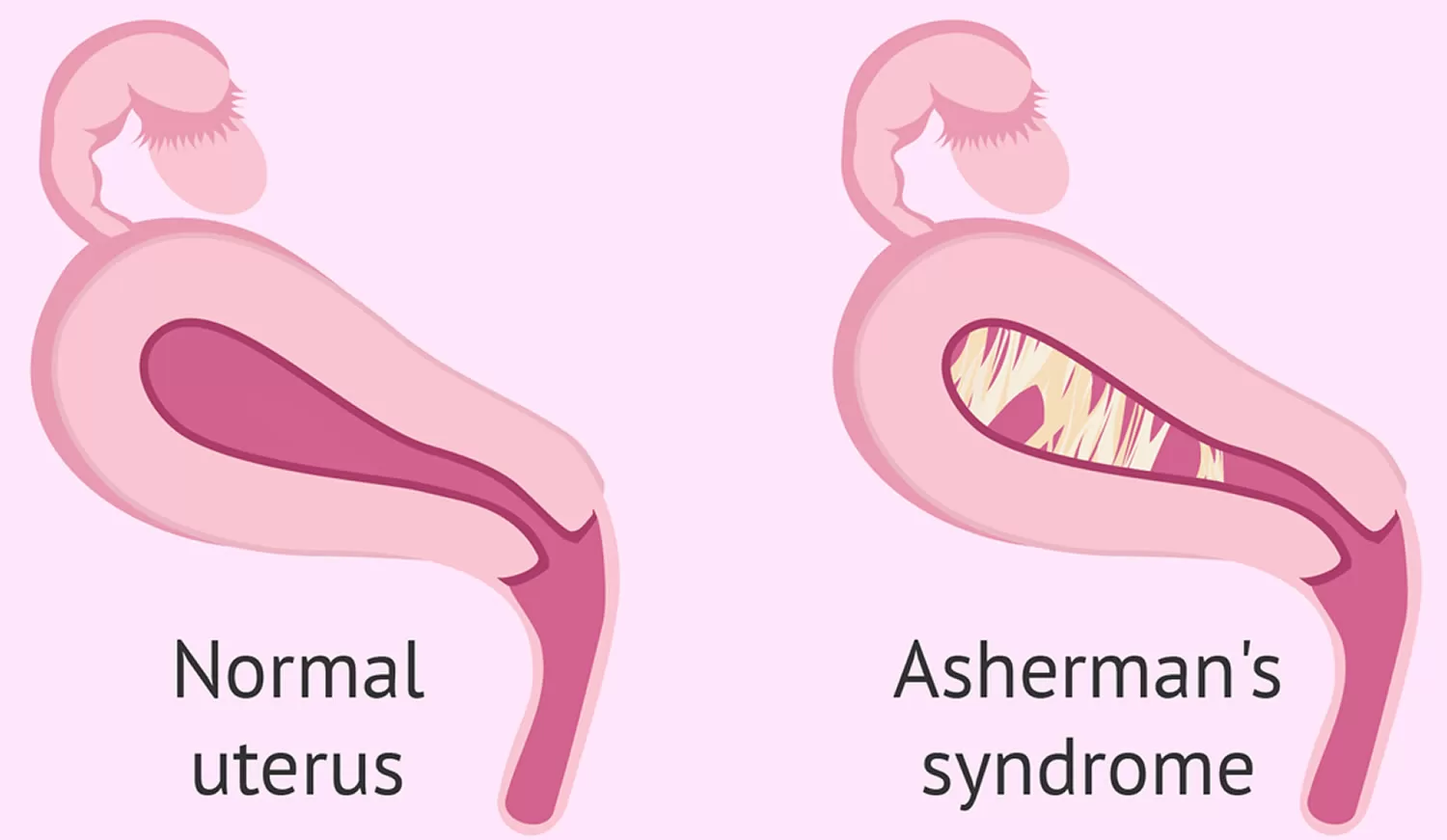
Asherman’s syndrome is an acquired condition where scar tissue (adhesions) form inside your uterus. The scar tissue can build up, decreasing the amount of open space inside your uterus. This condition can be a complication of medical procedures or cancer treatments. Women with Asherman’s syndrome may experience light or no periods, pelvic pain or infertility.
What is Asherman’s syndrome?
Asherman’s syndrome is a rare condition where scar tissue, also called adhesions or intrauterine adhesions, builds up inside your uterus. This extra tissue creates less space inside your uterus. Think of the walls of a room getting thicker and thicker, making the space in the middle of the room smaller and smaller.
This condition can cause pelvic pain and abnormal uterine bleeding and can lead to fertility issues. Asherman’s syndrome can be treated and treatment often helps relieve your symptoms.
How common is Asherman’s syndrome?
Asherman’s syndrome is considered a rare disease. It’s hard to know exactly how many people have Asherman’s syndrome because it can go undiagnosed. Some people may not experience any symptoms from this condition. If you don’t experience symptoms, you may never see a healthcare provider.
Who gets Asherman’s syndrome?
Asherman’s syndrome is an acquired condition, which means that something usually happens that causes you to develop scar tissue. You can acquire Asherman’s syndrome in several ways, including surgery, infections and cancer treatments.
Your risk of developing Asherman’s syndrome can increase if you’ve:
- Had surgery on your uterus in the past, including operative hysteroscopy, complicated dilation and curettage (D&C) or cesarean section (c-section).
- Had a history of pelvic infections.
- Been treated for cancer.
Is Asherman’s syndrome genetic?
Asherman’s syndrome is generally not a genetic condition. This means that you get this condition through something that happens (as a side effect of surgery, treatment or infection) and not passed down through your family.
What are the symptoms of Asherman’s syndrome?
If you have Asherman’s syndrome, you can experience a variety of symptoms. These symptoms can include:
- Having very light periods (hypomenorrhea).
- Not having a period (amenorrhea) or having abnormal uterine bleeding.
- Feeling severe cramping or pelvic pain.
- Having difficulty getting pregnant or staying pregnant.
In some cases, you may not experience any symptoms of Asherman’s syndrome. You may also still experience normal periods. If you feel any discomfort in your pelvis or have unusual periods, reach out to your healthcare provider.
What causes Asherman’s syndrome?
Asherman’s syndrome happens when scar tissue (adhesions) build up inside your uterus, limiting the space inside your uterus and sometimes blocking your cervix. This can happen for several reasons, but one of the main causes is often surgery of your uterus or cervix.
The causes of Asherman’s syndrome can include:
- Operative hysteroscopy: A surgery where your provider places a camera into your uterus and then cuts off and removes fibroids using an electric instrument.
- Dilation and curettage (D&C): A type of surgery, dilation and curettage (D&C) is used to open your cervix (dilate) and then remove tissue from your uterus. This tissue can be the lining of your uterus (endometrium) or tissue from a miscarriage or abortion. During the procedure, a tool is used to scrape away the extra tissue. This typically doesn’t cause scarring unless you have an underlying infection.
- Cesarean section (c-section): This surgery is used to deliver a baby. In some cases, a c-section can cause scar tissue to form. This can happen where the stitches (sutures) were used to stop bleeding (hemorrhages) during the c-section and you have an infection at the time of the procedure. Otherwise, it’s very rare for a c-section to cause Asherman’s syndrome.
- Infections: Infections alone don’t typically cause Asherman’s syndrome. But, when you have an infection while you undergo uterine surgery, like a D&C or a c-section, you can develop Asherman’s syndrome. Some infections that could lead to Asherman’s syndrome include cervicitis and pelvic inflammatory disease (PID).
- Radiation treatment: Sometimes, a treatment option can cause scar tissue to develop in your uterus. Radiation therapy can be used on conditions like cervical cancer, but this can cause adhesions (scar tissue) that lead to Asherman’s syndrome.
Can an IUD cause Asherman’s syndrome?
An intrauterine device (IUD) is a type of long-term birth control that’s placed inside your uterus and left there for a period of time (often several years). When this device is placed in your body, there’s always the risk of infection and the development of scar tissue. However, this isn’t a proven cause of Asherman’s syndrome and IUDs are not commonly linked to the condition.
How is Asherman’s syndrome diagnosed?
Asherman’s syndrome is typically diagnosed when you either experience symptoms of the condition like pelvic pain, amenorrhea (lack of menstruation), abnormal uterine bleeding or an inability to get and stay pregnant. Your medical history can also lead to a diagnosis of Asherman’s syndrome. If you have had a dilation and curettage (D&C) procedure, c-section, radiation therapy or pelvic infection, you may be tested for Asherman’s syndrome. All of these procedures and conditions can lead to Asherman’s syndrome.
During an appointment, your healthcare provider will go over your medical history. If you have had any kind of pelvic surgery that isn’t included in your medical history, make sure to tell your provider. That information can be very important in diagnosing Asherman’s syndrome. Your provider will then do a physical exam, but to detect scar tissue inside your uterus, your provider will perform a sonohysterogram. For a sonohysterogram, your provider injects a little saline solution inside your uterine cavity through a small catheter. Then, they use transvaginal ultrasound to see if any tissue is blocking the cavity or cervix.
What imaging tests can be used to diagnose Asherman’s syndrome?
Imaging tests allow your healthcare provider to see your internal organs. Different tests provide various amounts of detail. These tests can be done on top of your skin and involve little to no preparation, or they can be more complicated procedures.
Imaging tests that can be used to diagnose Asherman’s syndrome include:
- Ultrasound: This type of imaging test uses sound waves to create a picture of your internal organs. An ultrasound can be done externally on your skin or internally with a transvaginal ultrasound. A thin wand is inserted into the vaginal during this version of the test.
- Hysteroscopy: During this procedure, your healthcare provider uses a thin tool with a camera on the end to look inside your uterus. This is inserted in your vagina and moved up through your cervix and into your uterus. Hysteroscopy allows your provider a very detailed look at the inside of your uterus. It can also be used to treat Asherman’s syndrome.
- Saline infusion sonography: This imaging test uses ultrasound along with a saline (a mixture of salt and water) solution to create a clear image of the inside of your uterus. The fluid expands your uterus so that your provider can see details of the shape and defects of your uterine cavity. This gives your provider a very detailed look at the inside and outside of your reproductive organs.
How is Asherman’s syndrome treated?
There are several ways to treat Asherman’s syndrome. During a conversation with your healthcare provider, it’s good to discuss how this condition makes you feel — including any pain you may experience — as well as your goals for future fertility. In some cases where a woman isn’t experiencing symptoms, a treatment option can actually be no treatment. However, if your plan includes future pregnancies, there are treatment options that can remove the scar tissue. Treatment can also help if you’re experiencing cramps or pelvic pain.
The main goal of treatment is to remove the scar tissue and restore your uterus to its original size and shape. Treatment for Asherman’s syndrome can help:
- Relieve pain.
- Restore your normal menstrual cycle (periods).
- Allow for the possibility of pregnancy if you’re pre-menopausal.
Your healthcare provider may use hysteroscopy to remove the adhesions in your uterus. During a hysteroscopy, your provider uses a thin tool called a hysteroscope to look inside your uterus. This tool can also be used to remove scar tissue. The hysteroscope is inserted into your vagina, through your cervix and into your uterus. Scar tissue is very carefully removed during this procedure. A possible risk of this procedure is damaging healthy tissue inside your uterus while removing the scar tissue.
Hormonal treatments (estrogen) may be paired with a small intrauterine catheter left inside your uterus for a few days after the hysteroscopy. This will reduce the risk of recurring scar tissue formation after the procedure. In fact, estrogen promotes healing of your endometrium (inner lining of the cavity) and the catheter provides a physical barrier between your anterior and posterior uterine walls, so that they don’t adhere to each other in the few days following the procedure for scar tissue removal. When an intrauterine catheter is inserted, you’ll be given antibiotics to prevent possible infections.